Open versus closed systems for vitrification of human oocytes and embryosReproductive BioMedicine Online01 March 2015 |
 Gábor Vajta is Honorary Professor of BGI Shenzhen, China and Adjunct Professor at Central Queensland Univer- sity, Rockhampton, Australia. He is director of a consulting company (http://www.gaborvajta.com), providing services in human and domestic animal embryology all over the world. He has authored more than 160 publi- cations (books, book chapters and peer-reviewed journals, with close to 8,000 citations), and peer-reviews most journals in the field of human and domestic animal reproduction. He is an Editorial Board member of Cellular Reprogramming. Main topics of his research include cryopreservation of embryos and oocytes, somatic cell nuclear transfer, and various aspects of mammalian embryo culture.
Gábor Vajta is Honorary Professor of BGI Shenzhen, China and Adjunct Professor at Central Queensland Univer- sity, Rockhampton, Australia. He is director of a consulting company (http://www.gaborvajta.com), providing services in human and domestic animal embryology all over the world. He has authored more than 160 publi- cations (books, book chapters and peer-reviewed journals, with close to 8,000 citations), and peer-reviews most journals in the field of human and domestic animal reproduction. He is an Editorial Board member of Cellular Reprogramming. Main topics of his research include cryopreservation of embryos and oocytes, somatic cell nuclear transfer, and various aspects of mammalian embryo culture.
Reproductive BioMedicine Online (2015), doi: 10.1016/j.rbmo.2014.12.012
The application of vitrification considerably improved the in- vitro and in-vivo development of cryopreserved blastocysts and oocytes, and opened new perspectives for extended embryo culture, single blastocyst transfer, blastocyst biopsy, and alternative ways for fertility preservation or oocyte donation, respectively (Arav and Natan, 2013; Chian et al., 2014; Schoolcraft and Katz-Jaffe, 2013; Vajta, 2013).
Currently used vitrification techniques, however , differ from each other in many technical details, including solutions, equilibration and dilution parameters, carrier tools, cooling, storage and warming methods (Vajta and Nagy, 2006). The wide variety of methods makes selection of the best technique difficult, and causes serious problems when cryopreserved samples are transferred between laboratories. One of the most fundamental differences classifies vitrification techniques into two methods: ‘open’ and ‘closed’. Although closed methods are intended to keep the samples physically separated from liquid nitrogen during the entire cooling, storage and warming procedure, open systems allow direct contact between the sample containing medium and liquid nitrogen (Bielanski and Vajta, 2009).
As liquid nitrogen may contain infective agents, direct contact could theoretically mean a possibility for infection and disease transfer. No such disease transfer has yet been reported, although an estimated 600,000 to 1,000,000 vitrified embryos or embryos derived from vitrified oocytes by using open systems have been transferred. At present, most embryos and oocytes are vitrified with open systems worldwide, indicating a higher overall efficiency and consistency, although only a few comparisons between the two approaches have been published.
During the past few years, the open versus closed debate has become the subject of emotionally charged confrontations in many forums, which have included various ethical, legal and financial issues. We have been active contributors to these debates, have commercial interests (please see declaration), and have published pioneering results in the field; therefore, our opinion may be slightly biased and subject to debate.
The main purpose of this review is not to stimulate debate, but to focus attention on aspects that have not been considered so far, facts and arguments that may considerably help to abandon thinking in rigid categories, and promote the formation of a consensus in this very important issue.
To achieve this goal, we have attempted to answer the following questions: (i) what is the exact definition of an open versus closed system? Is the border evident and sharp? Are devices advertised as ‘closed’ always closed and always safe (i.e. free of danger of contamination from nitrogen or other sources)? (ii) what is the theoretical and practical risk of disease transmission via liquid or vapour phase nitrogen mediated infection? (iii) are closed systems as efficient as open ones for both human blastocyst and oocyte cryopreservation? (iv) what ethical and legal issues should be considered in selecting the appropriate procedure? and (v) what measures can be implemented to minimize sample infection and eliminate the possibility of cross-contamination to decrease or disclose even the theoretical danger of liquid or vapour phase nitrogen mediated disease transfer?
For most embryologists, the two categories are easily distinguishable. Open systems allow and closed systems eliminate direct contact between the sample-containing medium and liquid nitrogen. Consequently, from a disease transmission point of view, open systems are unsafe, and closed systems are safe.
The situation, however, is much more complicated.
The principle of vitrification in cryobiology is to eliminate totally ice formation in the medium that contains the sample, in all phases (cooling, storage and warming) of the procedure (Rall and Fahy, 1985). It can be achieved either by increased cooling and warming rates, or increasing concentration of cryoprotectants; in practical situations, both approaches are applied. The higher the cryoprotectant concentration, the lower the cooling rate required and vice versa. As highly concentrated cryoprotectants may cause toxic and osmotic injury, the preferred strategy is to use the highest possible cooling and warming rates, then to apply the lowest concentration of cryoprotectants that ensures safe ice-free solidification under these circumstances (Fuller and Paynter, 2004; Kasai and Mukaida, 2004; Stachecki and Cohen, 2004; Vajta and Nagy, 2006). High cooling and warming rates may also help to avoid chilling injury (Ghetler et al., 2005).
The easiest way to achieve high cooling and warming rates is to use the smallest solution volume and the highest temperature conductivity between the sample-containing medium and the cooling or warming agent, preferably liquid nitrogen for the former purpose (Arav, 1992).
Decreasing the thickness of the wall of the sample- holding container, for example straw, may be helpful. Obviously, a total elimination of the thermo-insulating layer is the best solution. However, the seemingly easiest approach - small droplets freely plunged into the liquid nitrogen (Landa and Tepla, 1990) - is suboptimal. To form a drop, an excessive amount (>3 l) of solution is required, and the nitrogen vapour coat that surrounds the warm medium will keep the drop for a relatively long period (8–10 s) over the surface of liquid nitrogen, decreasing considerably the cooling rate. Accordingly, carrier tools were introduced to hold small amounts, and ensure rapid submersion and fast elimination of the vapour coat (Martino et al., 1996; Steponkus et al., 1990). The small (>1, > 0.5 l) amount of solution also helps to minimize the danger of heterogenous ice formation (Rall et al., 1987).
Most carriers are based on homemade, simple tools, later modified for industrial production; however, these modifications did not always increase practical value and safety. At least 30 different carrier tools have been published, and at least 15 versions are commercially available. Most of them are slightly modified versions of the initially introduced carrier tools, such as the Open Pulled Straw (OPS) (Vajta et al., 1998a), the Cryoloop (Lane and Gardner, 2001; Lane et al., 1999), and the Cryotop (Hamawaki et al., 1999). All these systems are open in the original form. Most claimed ‘closed’ systems are the results of the modifications of these open systems.
A thorough structural and functional investigation of the existing vitrification systems reveals various levels of openness, consequently various levels of biosafety (differences that are commonly disregarded in the laboratory practice). ‘Safety’ or ‘biosafety’ in the context of this discussion refers to a theoretical danger of contamination that has been supported by some indirect evidence obtained in some analogous situation; it should not be confused with a proven, existing danger of cross-contamination and disease transmission.
Fully open systems include the unprotected OPS (Vajta et al., 1998a); tools using the Cryotop principle (i.e. the original Cryotop) (Hamawaki et al., 1999), Cryotech (Gutnisky et al., 2013), Cryolock (Garcia et al., 2011), Cryoleaf (Chian et al., 2009), Vitri-Inga (Almodin et al., 2010) with unsealed protective straws; and the Cryoloop stored in cryotubes. By applying these systems, samples contact liquid nitrogen directly during cooling, and are not safely protected from further contact and potential cross-contamination during storage. On the other hand, both cooling and warming rates can be extremely high (Bielanski and Vajta, 2009; Parmegiani and Vajta, 2011; Parmegiani et al., 2012b).
All systems mentioned in the previous paragraph above may belong to this group if after cooling, the carrier tool is inserted into a pre-cooled sterile container that is heat- sealed and capable to resists the extreme temperature changes (Vajta et al., 1998b). Some commercially available systems, for example the OPS and the recent version of Cryotop (Cryotop SC; http://www.kitazato.co.jp/biopharma/Cryotop2 .htmld), offer appropriately designed container straws for this purpose. The cooling and warming rates are as high as in the previous group; there are no indications that a properly performed wrapping procedure decreases survival or in-vitro or in-vivo developmental rates.
Semi-closed cooling connected to either open or closed storage systems. In these systems, the vitrification is carried out on the surface of a metal block that is half-submerged into liquid nitrogen (Cryohook; http://www.cryologic.com /cvm.htm) or inside of a container straw half-submerged into liquid nitrogen (Rapid I) (Larman and Gardner, 2011). In both systems, the presence of nitrogen vapour is unavoidable; accordingly, the possibility of nitrogen vapour-mediated contamination (Grout and Morris, 2009) cannot be excluded. These systems, despite some claims, are neither closed nor entirely biosafe. Cooling rates may be high on metal surfaces and somewhat compromised in vapour cooling; warming rates may be identical with those achieved in the previous groups.
In closed thin walled narrow capillaries, including the Cryotip (Kuwayama et al., 2005a) and the Cryopette (Parmegiani et al., 2012a), the device is heat sealed before cooling, and opened only after warming. Safety is compromised afterwards. At warming, these devices are immersed in a water bath, then the straws are cut and expelled into the appropriate medium. The manufacturer guideance (http://www .irvinescientific.com/uploads/technical-documentations/ 10397R_Cryotip-Tip-and-Tricks_Rev1.pdf; http://www .youtube.com/watch?v=gJcjdGMkhOY) for Cryotip and Cryopette, respectively, fail to suggest any decontamination measures after immersion after warming, and the surface remains contaminated (theoretically) from the liquid nitrogen, and (definitely) from the non-sterile water bath. Accordingly, when straws are opened with cutting devices (manuals do not suggest decontamination of these devices, either), the infection may freely propagate to the content. Investigators describing work with these devices do not mention this potential contamination source and do not describe any measures to prevent infection (Panagiotidis et al., 2013; Papatheodorou et al., 2013). Although currently available methods, such as wiping the surface of the capillary with ethanol or similar agents, decrease the chance of contamination, they are not 100% safe (see discussion below). Therefore, the safety of these seemingly closed systems is compromised at the final phase. Additionally, compared with previous groups of devices, a decrease in cooling and warming rates may occur, and the dilution of cryoprotectants after warming is delayed significantly.
Carrier tools sealed into a container, which separates them safely during cooling, storage and warming, was first outlined by Kuleshova and Shaw (2000), and used later with the OPS (Isachenko et al., 2006), high security vitrification kit (Abdelhafez et al., 2011), and Vitrisafe (Vanderzwalmen et al., 2009). These devices may offer the highest protection during the entire vitrification process. From a contamination point of view, they may even be safer than sealed straws used for traditional freezing. They may, however, seriously compromise cooling rates (Vanderzwalmen et al., 2009).
In summary, of the five currently available groups of vitrification tools described above, one is usually referred to as ‘open’ and four as ‘closed’. In contrast, devices in groups 1 to 4 do not prevent liquid nitrogen or contamination mediated through nitrogen vapour. Group 4 devices also expose embryos and oocytes to an additional danger of contamination from the warming water and cutting devices (Parmegiani et al., 2011). Only the last group, a relatively rarely used vitrification approach, can be regarded as safe from the point of liquid nitrogen mediated contamination, but the cooling rate may become compromised in this group.
The risk of disease transmission via liquid and vapour phase nitrogen-mediated infection has been discussed in detail (Bielanski and Vajta, 2009). As no new relevant data have since been published, the most important points are summarized here; for details and sources we refer to the above mentioned paper.
Exposure to low temperatures, with or without the use of cryoprotectants and sophisticated cryopreservation strategies, may or may not decrease the viability of infective agents. Survival depends on the species, complexity and size, and the way these agents are exposed to low temperatures. Unfortunately, methods purposely developed for cryopreservation of mammalian oocytes and embryos may also support cryosurvival of different kinds of microorganisms.
Liquid nitrogen, and also vapour phase nitrogen (Grout and Morris, 2009) may act as a vector between two contaminated samples. The phenomenon has been observed in the food industry , in dermatology , and also, under experimental conditions, during storage of semen pellets and artificially infected samples stored in an open vitrification device. The only published human infection clearly attributable to liquid nitrogen mediated cross-contamination occurred between large amounts of blood samples stored in leaky plastic containers (Tedder et al., 1995). In reproductive biology, including mammalian and human assisted reproduction, no disease transmission caused by liquid nitrogen mediated cross-contamination, or other cryopreservation-related source, has been reported. This finding is even more surprising in view of the following facts:
collection of semen is not a sterile procedure;
oocytes are contaminated with blood during collection;
many containers are inappropriately sealed or closed by
non-hermetical methods;
the outer surface of straws and vials is always infected;
storage tools (canisters, holders) are not sterilized;
openings of dewars mix air with LN2 vapour and may cause
infection;
factory derived LN2 is usually not transported under aseptic
conditions, and, accordingly, cannot be regarded as sterile, even if during production the infective agents are usually destroyed;
contaminated samples (sperm cells, oocytes) cannot be decontaminated;
in most IVF laboratories, dewars are not decontaminated regularly; acordingly, LN2 tanks and LN2 in tanks should always be regarded as contaminated.
Obviously , hermetically sealed containers may provide appropriate protection against infection during (and as a consequence of) storage. In practice, however, this protection is insufficient for most stored samples, regardless of the method used (traditional freezing or vitrification) and regardless of the applied devices (except for those belonging to Groups 2, 3 and 5, see the previous chapter). The reasons for potential cross contamination are as follows:
The only completely safe method for hermetical closing of containers is heat-sealing. Cotton plugs, beads commonly used for sperm, seemingly waterproof mechanical closures including screwed caps of cryovials or protective caps of several vitrification devices do not provide appropriate protection.
Taking into consideration all the possibilities of infection of the cryostored sample, the fact that no infection attributable to the cryopreservation procedures has yet been reported is rather surprising. The low incidence of infections, however, is applicable to all assisted reproduction techniques, independently of cryopreservation, and has been observed in both humans and domestic animals. No evidence is available that reproductive samples, including sperm, eggs, or embryos, can retain any blood-born pathogens by the time they are cryopeserved. Semen wash and IVF is a standard technique for procreation in couples discordant for a blood-born infection. No single infection after assisted reproduction techniques with processed reproductive samples has been reported to date (Savasi et al., 2013; Vitorino et al., 2011).
The most feasible explanation is that the threshold level required to cause a clinical infection is high in the female reproductive tract (probably as a natural protection against infective agents relatively abundant in the semen), and washing– dilution procedures during routine assisted reproduction techniques usually dilute the infective agents far below this level.
Even if the probability is extremely low (the estimated >500,000 transfers after the use of fully open (Group 1) vitrification systems did not result in a single detected infection, ie. the probability seems to be less than 0.0002%), measures to eliminate even the theoretical possibility should be implemented, by carefully considering the appropriate balance between the risks and benefits.
As traditional freezing has been successfully applied for decades for pre-compaction stage human embryos, the introduction of vitrification has resulted in breakthroughs in two main areas: cryopreservation of blastocysts and MII phase oocytes. These initial successes have been achieved with fully open systems belonging to Group 1, predominantly with the Cryotop (Kuwayama et al., 2005b) and Cryoloop (Lane and Gardner, 2001). Methods belonging to the closed systems (Groups 2, 3, 4 and 5) were mostly introduced 4–6 years later, except for the Cryotip, but were never really designed to be used for MII phase oocytes by the inventor (Kuwayama et al., 2005a), and most vitrification work is still carried out with the use of fully open systems.
Concerns about disease transmission related to vitrification were published as early as in the 1990s, and producers of various ‘closed’ or ‘safe’ systems have claimed no compromised results compared with the open counterparts; it is, however, surprising that, to date, the number of prospective randomized clinical trials proving these statements is extremely low (as far as we know two, from the same research group, listed below), and no multicentre studies have yet been published.
In 2013, two papers from the same group (Panagiotidis et al., 2013; Papatheodorou et al., 2013) have published two progressive randomized-controled trials comparing open and closed (Vitrisafe, Group 5) vitrification systems for cryopreservation of human blastocysts and oocytes, respectively. For blastocysts, no difference was found between the two systems in any parameters, including live birth rates. After oocyte vitrification, the only difference was the significantly lower survival rate by using the fully closed system (83 versus 91%). This difference, however, may have considerable consequence to overall efficiency.
Earlier publications include an observational study in an oocyte donation programme conducted in Cryo Bio System closed straw vitrification system (Group 5) versus open device. Stoop et al. (2012) found 90% survival; of those, 78% fertilized, and of those 34% found of excellent quality on day 3. Only these embryos were transferred, with high ongoing pregnancy and implantation rates. Although the investigators evaluated their results as excellent, the experimental design (transfer on day 3, with strongly selected group of embryos) did not allow comparison with those of other groups, neither in vitro, nor in vivo.
Earlier publications have been summarized in a recent review (Vajta, et al., 2013). Of the 93 papers analysed, 14 dealt with and blastocyst vitrification using open systems, and three used closed systems. The overall tendency was a slightly compromised outcome with closed systems, but the diverse approaches did not allow statistical analysis. For human oocytes, however, the 18 papers dealing with open systems reported obviously higher overall efficiency than the two using closed systems.
According to the impression of authors, most human IVF laboratories use open vitrification systems for embryos, and the overwhelming majority of those performing oocyte vitrification successfully use exclusively open systems (Groups 1 or 2). Many of these laboratories have tested closed systems (including those now reported by the above papers as successful), but the inferior results discouraged them. Some of these laboratories are concerned about publishing any comparisons because they do not want to be regarded as advocates of open systems and bear the possible financial and legal consequences (discussed later). None of these laboratories, however, use open systems to deliberately or inadvertently expose embryos, oocytes and patients (and indirectly their team) to potential harm, but use them because they are unable to find an appropriate alternative for the given purpose.
Both papers claiming clinically acceptable results after the use of a closed system for oocyte vitrification (Papatheodorou et al., 2013; Stoop et al., 2012) used completely closed (Group 5), (i.e. safe systems for the purpose). The cooling rate in these systems is compromised, whereas the warming rate is the same as that of an open system, indicating the principal importance of the latter. The experimental evidence cited by both papers to support this opinion, however, seems to be insufficient, so far. Seki and Mazur (Mazur and Seki, 2011; Seki and Mazur, 2008, 2009) used mouse oocytes that may have different cryobiological features from the eggs of humans. Moreover, the best survival rates reported in these studies were between 70 and 85%, whereas survival of 98% or above was reported after mouse oocyte vitrification by others (Gomes et al., 2008; Wang et al., 2009; Yan et al., 2010); limited efforts have been made to follow up developmental competence in vitro and in vivo, and most analysis is based on morphological survival. Accordingly, these achievements cannot be used as arguments against the need for open systems for human oocyte cryopreservation.
In summary, evidence supporting the suitability of closed systems for oocyte vitrification is scarce compared with the vast amount of published and unpublished excellent results with open systems. Studies of closed systems have been published by isolated research groups, resulting in only 13 reported births and 20 ongoing pregnancies in total (Papatheodorou et al., 2013; Stoop et al., 2012), whereas tens of thousands of healthy babies have been born worldwide during the past 8 years with the open systems. Right now, closed systems should be regarded as experiemental, and extensive work including multicentre prospective randomized trials, are still required to explain why these procedures are successful when applied in one laboratory and inefficient in others, and to prove that the suggested methods are really competitive alternatives to open systems.
The recent Guideline of the American Society for Reproductive Medicine regarding human metaphase II phase oocyte cryopreservation (2013) states that ‘there also are theoretic infectious disease concerns with the use of open vitrification methods. However, infectious transmission has never been observed in reproductive tissues from this technique’. The guideline concludes that ‘this technique (i.e. mature oocyte vitrification) should no longer be considered experimental’. As cited results were achieved by using open systems, the guideline supports their application.
In most countries, including many US states, and most European Union member countries, infertility is regarded as a medical condition. This is recognized by funding treatment, or by providing other benefits; even the lack of support, however, does not mean lack of acknowledgement, as illustrated by the lack of support of an obvious medical condtion, dental care. Infertility is a medical problem that should be treated by health professionals and the procedures supervised by health authorities.
The often emphasized ‘primum nil nocere’ principle, although not part of the Hippocratic Oath, is one of the basic laws of medicine. As all medical intervention means a certain risk to the patient, this principle should only be applied with great consideration to a given situation; and should not be an excuse to abstain from providing the required help. In contrast, it is the duty of the health service provider to make the right decision between the possible benefits and the chances of harm.
The US Preventive Services Task Force lists 5 levels of Strength of Recommendations for a medical intervention (http://www.uspreventiveservicestaskforce.org/3rduspstf /ratings.htm) (Table 1).
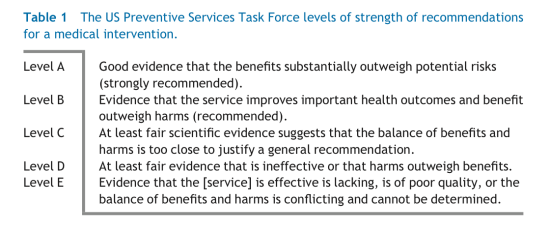
With vitrification of human oocytes, there is little doubt that the most used open systems (Group 1 and 2) applied worldwide with great success (in many laboratories the results are equal with those with fresh oocytes) substantially outweigh potential risk, and fall into Level A (strongly recommended).
Obligation to provide the best available treatment, however, is not restricted to life-treatening conditions; it is not just a moral duty, but a legal responsibility. According to the definition of medical malpractice or medical negligence, it occurs (among others) when a healthcare provider fails to provide adequate treatment for his or her patient. The consequences may be serious: loss of the possibility of having children.
The legal status of vitrification is controversial world- wide. In most developed countries, a general law has prevented the use of any procedures and tools that may cause infection or disease transmission. In these countries, authorities may have the right to enforce a full ban of any open vitrification systems because of the experimentally proven danger of disease transmission. According to a world- wide informal survey, with contributions from 41 scientists from 30 countries through Embryo Mail in 2011 (Vajta, unpublished), no definite law has been enforced in any of these countries, although scientists may feel the Sword of Damocles over their head.
Exmples of the relative tolerance and inactivity of authorities are as follows: (i) in many countries, including the USA, it is not entirely clear which authority is entitled to intervene; (ii) in many countries, authorities do not want to apply a general rule to a specific method that is working without problems in many laboratories, because they feel their duties fulfilled with declaration of the general rule (in case an infection happens), but do not want to interrupt a successful medical intervention; and (iii) the debate between scientists, companies, systems, tools, arguments, theoretical and real dangers is confusing, and many authorities do not want to destroy their reputation by making unreasonably strict restrictions; they are also influenced by the opinion of leading scientists in the field. According to the abovementioned survey, only three scientists of the 41 wanted a strict legal ban for the direct contact between the sample and liquid nitrogen. The majority have suggested tolerance, and authorities may accept this opinion.
One important legal and practical aspect of present-day vitrification methods is almost always disregarded: work safety issues in the embryo laboratory. Although hundreds of papers have been published on the theoretical possibility of cross- contamination, the potential hazard for scientists when working with currently available vitrification methods has been neglected. The issue has been summarized in a recent review (Vajta, et al., 2013). In fact, the primitive tools and approaches developed by vitrification pioneers 2 or 3 decades ago are still in use. Some companies offer more attractive looking, slightly increased practicality, but almost unchanged low safety. The actual way embryologists perform vitrification in all embryo laboratories does not meet any work safety regulations describing extreme (and fully justified) caution when working with liquid nitrogen. Injuries including superficial skin irritation, deep and irreversible tissue freezing, loss of sight, or even death caused by large amounts of liquid nitrogen stored in an unventillated room may occur any time, and some – including death – have already occurred in embryo laboratories. Unfortunately, currently available techniques simply cannot be performed in a safe way, but it is our duty to alert embryologists to take extreme care, and to draw the attention of companies to consider very seriously these aspects in their future products.
Disease transmission (which has not occurred to date) may theoretically be the result of contamination at cooling, storage and warming.
Storage is the most dangerous part from this perspective. Fortunately, it is the issue that has been mostly resolved, at least to the level of traditional freezing. Also, both open and closed vitrification systems may completely eliminate cross-contaimination by hermetically (heat-) sealed containers as described for Groups 2, 4, 5 and some systems belonging to Group 3. Some carriers from Group 1 have been upgraded by manufacturers to ensure hermetical cryostorage after vitrification, including OPS (Vajta et al., 1998b), or Cryotop SC. Alternatively, a double bagging hermetical system for safe storage can be conducted for any carrier (Parmegiani and Rienzi, 2011). Vapour phase storage systems with open devices (Cobo et al., 2010) may decrease, but cannot completely eliminate the risk of cross-contamination.
Warming can be also safely carried out without any danger of liquid nitrogen or nitrogen vapour contamination when Groups 2, 5, and hermetically stored Group 3 systems are used. In fact, the safety of warming with these tools is much higher than that in traditional freezing, as there is a secure way to avoid any contact between the contaminated surface of the outer container and the holding device. Additionally, the warming rate is not compromised and can be maintained optimally. As previously mentioned, for Group 4 devices, the warming means a definite and considerable infection hazard, and the procedure is prolonged by delaying dilution, and exposing fragile post-vitrification embryos and oocytes to the concentrated vitrification solution for a disproportionally long period.
The most critical phase is the cooling. The only safe way to avoid this danger is to use devices from Group 4 and 5, which also means compromised cooling rates, controversial consequences for Group 5, and problems with warming for Group 4.
In Groups 1, 2 and 3, there is a slight danger of contamignation at cooling. This danger, however, can be easily minimized using the following methods: (i) if factory-derived liquid nitrogen is stored separately and used exclusively for cooling, the danger of infection is minimal, and human immunodeficiency virus and hepatitis B infection is negligible, as these are not airborne viruses (Bielanski and Vajta, 2009); (ii) if liquid nitrogen (or vapour phase liquid nitrogen) is sterile filtered with disposable filters (Vajta et al., 1998b), large-capacity industrial devices, or by exposure to ultraviolet light (Parmegiani et al., 2009); and (iii) tools or vessels that contact liquid nitrogen (but not with the samples or sample-containing solutions) can be decontaminated easily by chemical agents, and flushed repeatedly with sterile distilled water (Bielanski and Vajta, 2009). According to a recent report, there is also an option of decontaminating samples with repeated flushing in sterile liquid nitrogen before warming (Parmegiani et al., 2012a).
Many leading laboratories have implemented one or two of these measures to prove their devotion towards measures to avoid liquid nitrogen or nitrogen vapour mediated cross-contamination. With the lack of any documented disease transfer, it is difficult to evaluate the need and efficiency of these measures, but they may help to maintain awareness and high laboratory standards.
In conclusion, the introduction and widespread application of vitrification is one of the most important achievements in human assisted reproducton techniques during the past decade, despite controversy and unclarified issues, mostly related to concerns about disease transmission. Thorough analysis of existing techniques has revealed that only a fraction of the so-called closed methods is really free of any possible sources of contamination, that neither open nor closed systems have so far resulted in any disease transmission. Overwhelming evidence shows that open systems are efficient for both blastocyst and oocyte vitrification; relevant data on closed systems, however, are sporadic, especially in the case of human oocytes, and far from convincing. A pragmatic approach in both legislation and scientific evaluation is suggested; in other words, consider the facts instead of theories, and acknowledge the value of methods that are used in thousands of clinics and have helped many infertile couples.
Abdelhafez, F., Xu, J., Goldberg, J., Desai, N., 2011. Vitrification in open and closed carriers at different cell stages: assessment of embryo survival, development, dna integrity and stability during vapor phase storage for transport. BMC Biotechnol. 11, 29.
Almodin, C.G., Minguetti-Camara, V.C., Paixao, C.L., Pereira, P.C., 2010. Embryo development and gestation using fresh and vitrified oocytes. Hum. Reprod. 25, 1192–1198.
Arav, A., 1992. Vitrification of oocytes and embryos. In: Lauria, A., Gandolfi, F. (Eds.), New Trends in Embryo Transfer. Portland Press, Cambridge, pp. 255–264.
Arav, A., Natan, Y., 2013. Vitrification of oocytes: from basic science to clinical application. Adv. Exp. Med. Biol. 761, 69–83.
Bielanski, A., Vajta, G., 2009. Risk of contamination of germplasm during cryopreservation and cryobanking in IVF units. Hum. Reprod. 24, 2457–2467.
Chian, R.C., Huang, J.Y., Gilbert, L., Son, W.Y., Holzer, H., Cui, S.J., Buckett, W.M., Tulandi, T., Tan, S.L., 2009. Obstetric outcomes following vitrification of in vitro and in vivo matured oocytes. Fertil. Steril. 91, 2391–2398.
Chian, R.C., Wang, Y., Li, Y.R., 2014. Oocyte vitrification: advances, progress and future goals. J. Assist. Reprod. Genet. 31, 411– 420.
Cobo, A., Romero, J.L., Perez, S., de los Santos, M.J., Meseguer, M., Remohi, J., 2010. Storage of human oocytes in the vapor phase of nitrogen. Fertil. Steril. 94, 1903–1907.
Fuller, B., Paynter, S., 2004. Fundamentals of cryobiology in reproductive medicine. Reprod. Biomed. Online 9, 680–691.
Garcia, J.I., Noriega-Portella, L., Noriega-Hoces, L., 2011. Efficacy of oocyte vitrification combined with blastocyst stage transfer in an egg donation program. Hum. Reprod. 26, 782–790.
Ghetler, Y., Yavin, S., Shalgi, R., Arav, A., 2005. The effect of chilling on membrane lipid phase transition in human oocytes and zygotes. Hum. Reprod. 20, 3385–3389.
Gomes, C.M., Silva, C.A., Acevedo, N., Baracat, E., Serafini, P., Smith, G.D., 2008. Influence of vitrification on mouse metaphase II oocyte spindle dynamics and chromatin alignment. Fertil. Steril. 90, 1396– 1404.
Grout, B.W., Morris, G.J., 2009. Contaminated liquid nitrogen vapour as a risk factor in pathogen transfer. Theriogenology 71, 1079– 1082.
Gutnisky, C., Alvarez, G.M., Cetica, P.D., Dalvit, G.C., 2013. Evaluation of the Cryotech Vitrification Kit for bovine embryos. Cryobiology 67, 391–393.
Hamawaki, A., Kuwayama, M., Hamano, S., 1999. Minimum volume cooling method for bovine blastocyst vitrification. Theriogenology 51, 165. Ref Type: Abstract.
Isachenko, V., Montag, M., Isachenko, E., Dessole, S., Nawroth, F., van der Ven, H., 2006. Aseptic vitrification of human germinal vesicle oocytes using dimethyl sulfoxide as a cryoprotectant. Fertil. Steril. 85, 741–747.
Kasai, M., Mukaida, T., 2004. Cryopreservation of animal and human embryos by vitrification. Reprod. Biomed. Online 9, 164–170. Kuleshova, L.L., Shaw, J.M., 2000. A strategy for rapid cooling of
mouse embryos within a double straw to eliminate the risk of contamination during storage in liquid nitrogen. Hum. Reprod. 15, 2604– 2609.
Kuwayama, M., Vajta, G., Ieda, S., Kato, O., 2005a. Comparison of open and closed methods for vitrification of human embryos and the elimination of potential contamination. Reprod. Biomed. Online 11, 608–614.
Kuwayama, M., Vajta, G., Kato, O., Leibo, S.P., 2005b. Highly efficient vitrification method for cryopreservation of human oocytes. Reprod. Biomed. Online 11, 300–308.
Landa, V., Tepla, O., 1990. Cryopreservation of mouse 8-cell embryos in microdrops. Folia Biol. (Praha) 36, 153–158.
Lane, M., Gardner, D.K., 2001. Vitrification of mouse oocytes using a nylon loop. Mol. Reprod. Dev. 58, 342–347.
Lane, M., Schoolcraft, W.B., Gardner, D.K., 1999. Vitrification of mouse and human blastocysts using a novel cryoloop containerless technique. Fertil. Steril. 72, 1073–1078.
Larman, M.G., Gardner, D.K., 2011. Vitrification of mouse embryos with super-cooled air. Fertil. Steril. 95, 1462–1466.
Martino, A., Songsasen, N., Leibo, S.P., 1996. Development into blastocysts of bovine oocytes cryopreserved by ultra-rapid cooling. Biol. Reprod. 54, 1059–1069.
Mazur, P., Seki, S., 2011. Survival of mouse oocytes after being cooled in a vitrification solution to -196 degrees C at 95 degrees to 70,000 degrees C/min and warmed at 610 degrees to 118,000 degrees C/min: a new paradigm for cryopreservation by vitrification. Cryobiology 62, 1–7.
Panagiotidis, Y., Vanderzwalmen, P., Prapas, Y., Kasapi, E., Goudakou, M., Papatheodorou, A., Passadaki, T., Petousis, S., Nikolettos, N., Veletza, S., Prapas, N., Maroulis, G., 2013. Open versus closed vitrification of blastocysts from an oocyte-donation programme: a prospective randomized study. Reprod. Biomed. Online 26, 470– 476.
Papatheodorou, A., Vanderzwalmen, P ., Panagiotidis, Y ., Prapas, N., Zikopoulos, K., Georgiou, I., Prapas, Y., 2013. Open versus closed oocyte vitrification system: a prospective randomized sibling- oocyte study. Reprod. Biomed. Online 26, 595–602.
Parmegiani, L., Rienzi, L., 2011. Hermetical goblets for cryostorage of human vitrified specimens. Hum. Reprod. 26, 3204–3205. Parmegiani, L., Vajta, G., 2011. Contamination of single-straw carrier for vitrification. Fertil. Steril. 95, e69.
Parmegiani, L., Cognigni, G.E., Filicori, M., 2009. Ultra-violet sterilization of liquid nitrogen prior to vitrification. Hum. Reprod. 24,2969.
Parmegiani, L., Cognigni, G.E., Bernardi, S., Cuomo, S., Ciampaglia,
W., Infante, F.E., Tabarelli de Fatis, C., Arnone, A., Maccarini, A.M., Filicori, M., 2011. Efficiency of aseptic open vitrification and hermetical cryostorage of human oocytes. Reprod. Biomed. Online 23, 505–512.
Parmegiani, L., Accorsi, A., Bernardi, S., Arnone, A., Cognigni, G.E., Filicori, M., 2012a. A reliable procedure for decontamination before thawing of human specimens cryostored in liquid nitrogen: three washes with sterile liquid nitrogen (SLN(2). Fertil. Steril. 98, 870–875.
Parmegiani, L., Cognigni, G.E., Filicori, M., 2012b. Vitrification carriers and European regulation. Fertil. Steril. 97, e24.
Rall, W.F., Fahy, G.M., 1985. Ice-free cryopreservation of mouse embryos at -196 degrees C by vitrification. Nature 313, 573–575.
Rall, W.F., Wood, M.J., Kirby, C., Whittingham, D.G., 1987. Development of mouse embryos cryopreserved by vitrification. J. Reprod. Fertil. 80, 499–504.
Savasi, V., Oneta, M., Parrilla, B., Cetin, I., 2013. Should HCV discordant couples with a seropositive male partner be treated with assisted reproduction techniques (ART). Eur. J. Obstet. Gynecol. Reprod. Biol. 167, 181–184.
Schoolcraft, W.B., Katz-Jaffe, M.G., 2013. Comprehensive chromosome screening of trophectoderm with vitrification facilitates elective single-embryo transfer for infertile women with advanced maternal age. Fertil. Steril. 100, 615–619.
Seki, S., Mazur, P., 2008. Effect of warming rate on the survival of vitrified mouse oocytes and on the recrystallization of intracellular ice. Biol. Reprod. 79, 727–737.
Seki, S., Mazur, P., 2009. The dominance of warming rate over cooling rate in the survival of mouse oocytes subjected to a vitrification procedure. Cryobiology 59, 75–82.
Stachecki, J.J., Cohen, J., 2004. An overview of oocyte cryopreservation. Reprod. Biomed. Online 9, 152–163.
Steponkus, P.L., Myers, S.P., Lynch, D.V., Gardner, L., Bronshteyn, V., Leibo, S.P., Rall, W.F., Pitt, R.E., Lin, T.T., MacIntyre, R.J., 1990. Cryopreservation of Drosophila melanogaster embryos. Nature 345, 170–172.
Stoop, D., De, M.N., Jansen, E., Platteau, P., Van den Abbeel, E., Verheyen, G., Devroey, P., 2012. Clinical validation of a closed vitrification system in an oocyte-donation programme. Reprod. Biomed. Online 24, 180–185.
Tedder, R.S., Zuckerman, M.A., Goldstone, A.H., Hawkins, A.E., Fieldting, A., Briggs, E.M., Irvin, D., Blair, S., Gorman, A.M., Patterson, K.G., Linch, D.C., Heptonstall, J., Brink, N.S., 1995. Hepatitis B transmission from contaminated cryopreservation tank. Lancet 346, 137–139.
Vajta, G., Reichart, A., Ubaldi, F., Rienzi, L., 2013. From a backup technology to a strategy-outlining approach: the success story of cryopreservation 2013. Expert. Rev. Obst. Gynecol. 8, 181–190.
Vajta, G., 2013. Vitrification in human and domestic animal embryology: work in progress. Reprod. Fertil. Dev. 25, 719–727.
Vajta, G., Nagy, Z.P., 2006. Are programmable freezers still needed in the embryo laboratory? Review on vitrification. Reprod. Biomed. Online 12, 779–796.
Vajta, G., Holm, P ., Kuwayama, M., Booth, P .J., Jacobsen, H., Greve, T., Callesen, H., 1998a. Open Pulled Straw (OPS) vitrification: a new way to reduce cryoinjuries of bovine ova and embryos. Mol. Reprod. Dev. 51, 53–58.
Vajta, G., Lewis, I.M., Kuwayama, M., Greve, T., Callesen, H., 1998b. Sterile application of the Open Pulled Straw (OPS) vitrification method. Cryo Letters 19, 389–392.
Vanderzwalmen, P., Ectors, F., Grobet, L., Prapas, Y., Panagiotidis, Y., Vanderzwalmen, S., Stecher, A., Frias, P., Liebermann, J., Zech, N.H., 2009. Aseptic vitrification of blastocysts from infer- tile patients, egg donors and after IVM. Reprod. Biomed. Online 19, 700–707.
Vitorino, R.L., Grinsztejn, B.G., de Andrade, C.A., Hokerberg, Y.H., de Souza, C.T., Friedman, R.K., Passos, S.R., 2011. Systematic review of the effectiveness and safety of assisted reproduction techniques in couples serodiscordant for human immunodefi- ciency virus where the man is positive. Fertil. Steril. 95, 1684– 1690.
Wang, Z., Sun, Z., Chen, Y., He, F., 2009. A modified cryoloop vit- rification protocol in the cryopreservation of mature mouse oocytes. Zygote 17, 217–224.
Yan, C.L., Fu, X.W., Zhou, G.B., Zhao, X.M., Suo, L., Zhu, S.E., 2010. Mitochondrial behaviors in the vitrified mouse oocyte and its par- thenogenetic embryo: effect of Taxol pretreatment and relation- ship to competence. Fertil. Steril. 93, 959–966.
Declaration: Gábor Vajta is co-owner of a company that produces OPS for research and commercial application. Laura Rienzi and Filippo Maria Ubaldi report no financial or commercial conflict of interest.
http://www.rbmojournal.com/article/S1472-6483(15)00005-X/fulltext

 (9)
(9)
5985